COVID-19 seasonality is primarily driven by low 25-hydroxyvitamin D levels in winter-spring
Just like influenza
There is a well-known seasonality of influenza in countries 30 degrees or more from the equator.
From Cannell et al. 2006: Epidemic influenza and vitamin D. (Redrawn from the original in Hope-Simpson 1981.) COVID-19 seasonality is much the same - it is caused primarily by moderate fluctuations in population average 25-hydroxyvitamin D levels.
[Update 2022-05-14: I have added some further diagrams and text at the end.]
Proper D3 supplementation can easily boost these levels, all year round, well above ordinary unsupplemented summer levels - to 50ng/ml 125nmol/L or more, which is what the immune system needs to function properly. This should be encouraged and supported for the entire population, on a voluntary basis, to generally attain 25-hydroxyvitamin D levels well above current average summer peaks.
COVID-19 transmission and severity is reduced by lockdowns, social distancing, vaccination and in some unfortunately rare cases, widely deployed early treatment - such as ivermectin in Uttar Pradesh . The impact of vaccination is complex and contentious, with rapidly waning protection from infection and transmission, and longer lasting protection from severe outcomes. High levels of long-lasting infection acquired immunity, such as in India (57.7% March to June 2021: page 4 Anand et al. 2021), also greatly reduce transmission and hospitalisation rates.
In countries 30° or more from the equator, COVID-19 transmission and severity follows a widely recognised seasonal pattern of transmission primarily in winter and spring. In equatorial countries, the monsoon, with its high humidity and rainfall, more time spent indoors and reduced sunlight, is also increases transmission of COVID-19 (Rahul KM and Lennart Kraft, 2021).
For background on vitamin D and COVID-19, please see my two previous articles 2021-09-05 and 2021-10-24 (proper vitamin D3 supplemental intakes) and the research articles cited at What every MD, immunologist, virologist and epidemiologist should know about vitamin D and the immune system: vitamindstopscovid.info/05-mds/ .
Mainstream media and a great deal of academic discussion on COVID-19 seasonality centres on temperature, humidity and people huddling indoors with closed windows. These discussions tend to ignore the influence of well-known seasonal fluctuations in 25-hydroxyvitamin D levels and the apparently little-known, but thoroughly established, relationship between low 25-hydroxyvitamin D levels and both weakened and hyper-inflammatory immune responses and so with increased transmission and severity of viral respiratory diseases such as influenza and COVID-19.
This almost ubiquitous failure to recognise the importance of vitamin D - right up to the highest levels of government policymaking - is perplexing to me and many other engineering types. We have not been subject to whatever lifelong constellation of factors it is which makes many or most members of the medical profession apparently quite blind, or at least extremely uninterested, in what to us is the obvious importance of vitamin D to the immune system.
This is a social and organisational behaviour problem which is far more complex than biochemistry, immunology etc. It is extremely exasperating and must be solved.
A mistake such as this, when made the majority of the world’s ~10 million doctors, is a single point of failure for which humanity has no workaround.
In this case, mainstream doctors’ collective past and current failure to understand the immune system’s need for good (50ng/ml or more) 25-hydroxyvitamin D has been a crucial element enabling and driving a global program by many governments which can most briefly be described as vaccine tyranny: Everyone (down to some ever-lower age) must get vaccinated. Then they will need boosters. We are vaccinating our way to freedom. Only the vaccinated will be able to go to shops other than supermarkets and pharmacies, indefinitely. (Announced 2021-10-24 here in Victoria, Australia.) There are no early (home, when first diagnosed) treatments. There are no ways of improving your immune system. If you develop hypoxia, come to hospital and we will give you oxygen, prednisone (dampens inflammatory immune responses and innate and adaptive antiviral responses) and other drugs. If these don’t cause you to recover, we will put you on invasive mechanical ventilation, from which you will be lucky to survive without lasting disability.
“Physicians and Vaccine Tyranny” is the name of a desperate, pleading, essay by an American doctor writing under a pseudonym: www.americanthinker.com/articles/2021/10/physicians_and_the_vaccine_tyranny_.html
The great majority of the wrangling about vaccines, transmission, severity, lockdowns, masks etc. is being done by people who have no understanding of how the immune system depends on vitamin D. Everyone knows that the UV-B in high elevation sunlight creates vitamin D3 in our skin. In countries far from the equator, everyone knows this happens in summer, but not in winter. Everyone knows that respiratory viruses, including influenza and SARS-CoV-2, are more transmissible and more likely to harm and kill in winter. However, not knowing that most people’s winter low vitamin D levels cripple their innate and adaptive antiviral immune responses, and drive the dysregulated hyper-inflammatory (destroying our own healthy cells) immune responses which cause severe COVID-19, most people think that the seasonal increase in infectivity is something to do with cold, wet outdoor conditions or more time spent indoors. However, people spend most of their time in vehicles and buildings all year round.
In vehicles and buildings, heating and air conditioning frequently reverses the seasonal changes in outdoor temperature and humidity. There are no convincing mechanistic explanations for why outdoors changes in temperature and humidity have such enormous effects on viral transmission and disease severity.
Mother Nature runs a vitamin D experiment on countries more than about 30°from the equator every year. As more and more people discover that the vaccines they placed their faith in are far less effective than promised - and less safe - I imagine that they will look at the seasons, the waves of COVID-19, the millions of deaths, the Sun - and eventually their thoughts will turn to vitamin D.
The diagram above was created in 1980 by Robert Edgar Hope Simpson (1908 - 2003 [Wikipedia]) - a GP with an extensive and varied career, especially regarding infectious diseases. He proposed solar radiation as the seasonal factor driving the observed patterns, but did not mention its effect on vitamin D.
The eight authors of Cannell et al. 2006 (three of whom are members of the Nutrition for Immune System Health - NISH - email discussion list I coordinate nish.groups.io) proposed that vitamin D was the primary or sole cause of this seasonality. This was five years before the Institute of Medicine (IOM) report which set the standards most governments and MDs rely upon to this day: 20ng/ml 50nmol/L 25-hydroxyvitamin D, to be attained by “adults” with 0.0125mg 600IU D3 a day.
The article I wrote yesterday: nutritionmatters.substack.com/p/government-vitamin-d3-supplementation recounts how the IOM ignored advice to set a standard of 25-hydroxyvitamin D repletion above 20ng/ml and made a huge error in its statistical analysis, which resulted in a terribly low 600IU/day recommended daily allowance for vitamin D3. Here, from Cannell et al. 2006, is an example of that advice:
Vitamin D supplementation should stabilize 25(OH)D concentrations consistent with levels obtained by natural summertime sun exposure (50 ng/ml) while avoiding toxic levels. Those with large amounts of melanin in their skin, the obese, those who avoid the sun, and the aged may need up to 5000 IU/day to obtain such levels, especially in the winter.
(In fact, more than 0.125mg 5000IU D3 is needed for people whose bodyweight exceeds 70kg - and obesity requires a still higher intake.)
If the IOM had accepted this advice that D3 supplementation should be sufficient to attain 50ng/ml circulating 25-hydroxyvitamin D, if doctors had accepted this and passed it on to the public and their patients, and if most people had followed this advice, there would be no COVID-19 pandemic. R0 in Wuhan would have been below 1.0. Numerous acute and chronic diseases would be far less prevalent.
Instead we have most of the population, in most countries with unsupplemented (and unboosted by recent UV-B skin exposure) 25-hydroxyvitamin D levels between 5 and 25ng/ml (7.5 and 62.5nmol/L).
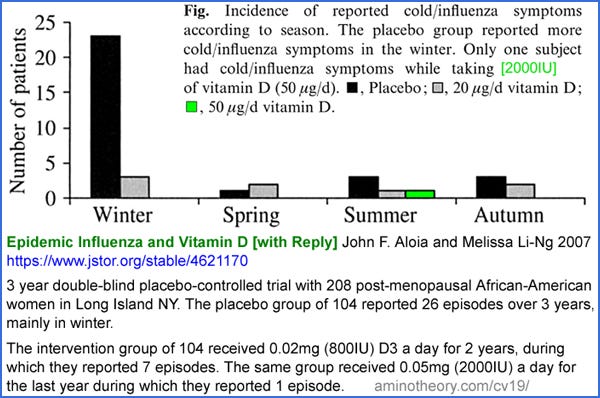
Cannell et al. wrote that the hypothesis should be tested. “Are patients with low 25(OH)D levels more likely to contract viral respiratory infections?”. This call was answered by Aloia and Li-Ng 2007 who reported on a beautifully designed, 3 year long, double-blind [WP], placebo-controlled [WP] RCT (randomised controlled trial [WP]) involving 208 post-menopausal African American women in Long Island, New York State, USA. This diagram explains the results:
In the intervention group, 0.02mg 800IU/day D3 resulted in 7 infections over two years (grey) with only a little more in winter, while placebo group (black) reported 26 episodes over three years, mostly in winter. In the third year, the same 104 women were given 0.05mg 2000IU/day D3 (green) and there was only one episode, in summer.
The very small supplemental intake of 800IU/day D3 greatly reduced influenza incidence, and abolished the concentration of cases in winter. Just 0.05mg 2000IU/day D3 pretty much abolished influenza for these women.
This is not the same as raising the 25-hydroxyvitamin D levels of whole populations of people, or of the great majority of a population. In this trial, the subjects were living in a generally unsupplemented community and so were at the currently normal risk of being exposed to influenza viruses, which is much higher in winter due to more people being infected then. This trial measured the ability of individuals to avoid symptomatic infection in a setting of unchanged viral insults.
If an entire population raised their 25-hydroxyvitamin D levels in the same way as the women in the intervention group, then we would expect still fewer infections, since all individuals would be less likely to develop symptomatic influenza, for any given viral insult, and this reduction in symptomatic cases would therefore reduce the average level of viral insult of all people in the population. This would further reduce the number of cases and this would still further reduce the average level of viral insult.
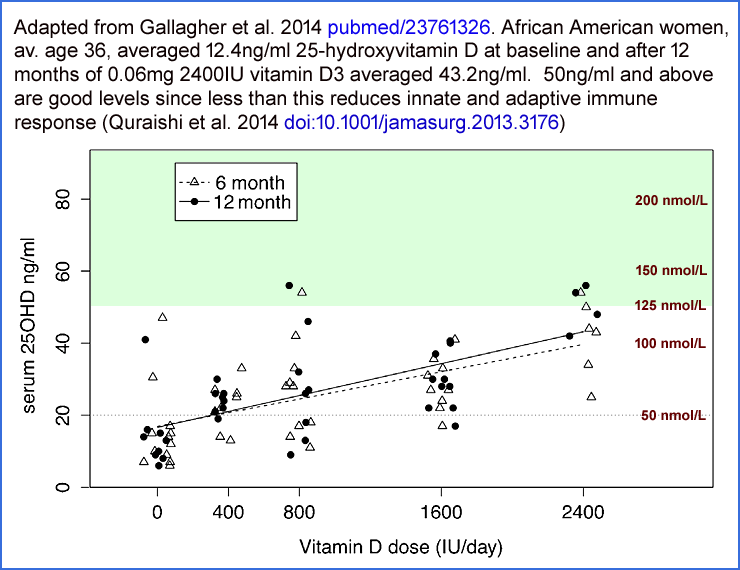
We don’t know the 25-hydroxyvitamin D levels of these women. However, it is reasonable to assume that the placebo group’s levels were around 10 to 15ng/ml and that intervention group’s levels averaged around 22ng/ml for the first two years (800IU/day) and around 38ng/ml for the third year with 2000IU/day. These are my guesstimates based on the following graph from Gallagher et al 2014:which depicts the 25-hydroxyvitamin D levels for five groups of African American women who were given zero, 0.01mg 400IU, 0.02mg 800IU, 0.04mg 1600IU and 0.06mg 2400IU D3 a day for 12 months. (The graph for white women shows about the same results for 2400IU, but less of a slope since their unsupplemented average level was about 22ng/ml.)
It is easy to imagine R0 (R nought, the basic reproduction number [WP] falling below 1.0 if a population of individuals, who all responded similarly to these test subjects, raised their 25-hydroxyvitamin D levels to about 38ng/ml. Below 1.0, there can be no epidemic [WP] or pandemic [WP] spread of the virus, since on average each person passes the disease on to less than one other person.
Common explanations for the seasonality of influenza, other viral respiratory diseases and COVID-19 include outdoors temperature and humidity, and people spending more time indoors in winter. However, most transmission occurs in buildings and vehicles and the time people spend in these hardly varies all year round.
One seasonal effect is summer's high UV-B levels inactivating viruses in aerosols and fomites (deposits on surfaces such as door handles) much faster than in winter. However, this is only true in daylight hours and for outdoor surfaces, since UV-B does not pass through glass.
Another likely significant factor is that in winter, building and vehicle air is recirculated more and has a lower relative humidity due to being heated. This is likely to causes respiratory droplets to dry into single virus particles which remain aloft much longer than the droplets would, at least compared to summer indoor conditions involving cooling and so lower relative humidity and/or more fresh air from open windows.
These two mechanisms are likely to contribute to the seasonality of viral respiratory infections such as influenza, various common cold viral infections - and of course COVID-19. Quantifying their importance would, in principle, be possible with very careful studies in tightly specified conditions. Extrapolating such quantitative findings to give a realistic understanding of their importance in a whole country would be largely guesswork.
Outdoor temperature and humidity are sometimes cited as causes of seasonality, but there are no convincing mechanistic arguments - and observational correlations are not so clear. In late December 2020 now-abandoned project to look at all such research, I started with the results of a 2020-10-05 preprint [WP] survey by Rahul Kalippurayil Moozhipurath (who goes by Rahul KM for short).
I extended Rahul’s survey of COVID-19 seasonality articles with the results of 8 others I found by 2020-12-23: Vinoj, Sfîcă, Ramirez, Finlayson, Isaia, Heibati, Walrand and Fontal. I guess I there are dozens more now, in late October 2021. Here is a screenshot which represents what I found:
This is not definitive. This explains how I came to believe that the seasonality research I found was inconclusive about (outdoors) humidity and rain while clearly supporting UV-B light as negatively correlating with COVID-19 transmission. Temperature is also less clearly negatively correlated, but high temperatures tend to correlate with high Sun illumination and lack of clouds - and so with UV-B.
Outdoors and away from home transmission is arguably more important for overall community transmission than the almost inevitable indoors transmission in homes and workplaces, but variations in outdoor conditions and in behaviour cannot, on their own, account for the strong observed seasonality.
With flu in equatorial regions, there is no winter or summer and no clear pattern in influenza or COVID-19 transmission. However, monsoonal periods reduce UV-B exposure for a few months, reduce temperatures a little and raise humidity. The waning immunity from previous flu infections leads to re-infection in local waves which are not strongly synchronised to the time of year in equatorial countries, compared to the strong synchronisation with winter-spring for countries 30 degrees or more from the equator, as clearly seen in the Cannell et al. graph.
Most people fail to consider the strong modulation of population average 25-hydroxyvitamin D levels away from the equator, due to seasonal variation in the angle of the Sun at midday and due to seasonal warm and hot daytime temperatures which drive behaviours which expose skin to direct sunshine in the middle of the day. The thermal mass of the top layers of the ocean cause peak atmospheric temperatures to lag the summer solstice by nearly 2 months. The D3 produced in outdoor summer activities creates 25-hydroxyvitamin D within days, which has a half-life of a month or two. So 25-hydroxyvitamin D levels broadly peak in August in the northern hemisphere and February in the southern. Sunlight earlier in the morning and later in the afternoon involves shallow angles and longer paths through the atmosphere, which more strongly attenuate the ~295nm UV-B which converts 7-dehydrocholesterol [WP] to D3. This light is at the highest frequency, shortest wavelength, end of the Sun’s spectrum.
Once it is understood that low 25-hydroxyvitamin D levels weaken immune responses and so greatly increase overall community transmission, it is easy to see that seasonal patterns of flu and COVID-19 transmission and severity are driven primarily by these levels - and only to a limited extent by the other mechanisms just mentioned. Low 25-hydroxyvitamin D levels weaken innate and adaptive responses to viruses and other types of pathogen, so there is:
A greater chance of being infected for any given viral insult - so there are more infected people for any general level of total viral shedding by however many people are infected.
A longer and more intense illness, which causes a longer and more productive period of viral shedding. This results in a greater total amount of viruses shed per infected person.
These two mechanisms multiply recursively in winter to greatly increase community-wide transmission rates, as well as the incidence of severe symptoms.
In the summer of 2020, with the original (or almost so) COVID-19 variant, hospitalisation rates (a better measure of transmission than PCR [WP] tests, which were beginning to be deployed widely) in the UK were dropping consistently for months. R0 was below 1.0 and the pandemic would have died out if nothing had changed.
This was in a period of summer high average population 25-hydroxyvitamin D levels. By the end of August, only 795 COVID-19 patients remained in UK hospitals. Two things changed. Firstly, as shown in the four wavy line BIOBANK historical 25-hydroxyvitamin D seasonal curves (from Raisi-Estabragh et al. 2020):
average 25-hydroxyvitamin D levels dropped. Secondly, the variant later known as alpha out-performed the original variant. Hospitalisations rose dramatically, and this chart from mid-December 2020 doesn't show how many more people were hospitalised that winter:
The summer of 2021 has not lead to such a decline in cases and hospitalisations, largely due to the more transmissible delta variant. However, the example of vitamin D suppression of COVID-19 transmission in the UK summer of 2020, before any vaccinations were conducted and while there were no lockdowns, is a stark demonstration of the sensitivity of transmission to even modest changes in relatively low average 25-hydroxyvitamin D levels. According to the BIOBANK data, peak summer average levels for Whites were still only half the 50ng/ml 125nmol/L needed for proper immune function: vitamindstopscovid.info/02-autocrine/#04-quraishi . Levels for BAME (Black, African and Minority Ethnic) people were much lower and less subject to seasonal variation, due to melanin-rich skin and/or sun avoidant clothing and lifestyles.
Average 25-hydroxyvitamin D levels in the UK at any time of year, even for fair-skinned people, are terribly low compared to the 50ng/ml 125nmol/L required for proper immune function, as can be seen in this chart:
which I prepared from the BIOBANK data from Sutherland et al. 2020: sci-hub.se/10.1016/j.clnu.2020.11.019 . Only 7% of Whites have more than 30ng/ml 75nmol/L in winter. But the real horror - the tragedy presided over for years by what MDs and the government supposedly working together to protect everyone's health - is the disastrously low 25-hydroxyvitamin D levels of those with melanin-rich skin. More than half of UK Asians (whose ethnic background is mainly from Pakistan, India and Bangladesh) have less than 10ng/ml 25nmol/L all year round!
These people's high susceptibility to COVID-19 infection, harm and death is known to all, but was generally explained as being due to large families, poor standard of living and the need to work in high transmission environments. These factors are likely significant, but the terrible toll among BAME doctors was not explicable in terms of low standard of living. With (according to the BIOBANK data) 90% of the UK Asian population having less then 20ng/ml 50nmol/L all year round, even a cursory understanding of the importance of vitamin D to the immune system provides a far more complete explanation for these people’s suffering, harm and death. This can be largely prevented, for all people, all year round, with D3 supplementation ten or more times more than the UK government's officially recommended 0.01mg 400IU/day.
We can’t know for sure, for any particular county, in winter, what level of 25-hydroxyvitamin D is required (assuming we generally raise it in almost all of the population) to suppress R0 below 1.0 with the delta variant - or whatever variants outperform it. However, for numerous health reasons, it is madness to have humans with generally less than 50ng/ml 25-hydroxyvitamin D - especially when trying to suppress COVID-19 transmission and severity.
While delta is significantly more transmissible than the mid-2020 variant, immune systems work so much better with 50ng/ml 25-hydroxyvitamin D than they do with current UK summer averages, which are probably half this, that it is reasonable to assume that a 50ng/ml 125nmol/L population average would suppress delta and likely future variants. The sooner we achieve this, for all humanity, the less chance there will be for more transmissible and/or more virulent variants to evolve.
[Update 2022-05-14]
Here are some additional items of interest.
Another chart demonstrates the strong winter seasonality of influenza in countries far from the equator. This is from:
Worldwide transmission and seasonal variation of pandemic influenza A(H1N1)2009 virus activity during the 2009–2010 pandemic
Aaron D. Storms et al. Influenza and Other Respiratory Viruses 2013-03-30
https://onlinelibrary.wiley.com/doi/full/10.1111/irv.12106
We know from multiple research articles that COVID-19 severity is inversely proportional to 25-hydroxyvitamin D levels. The same is generally true of many diseases, including influenza. It is reasonable to assume that the total amount of viral shedding which occurs scales with disease severity. The length of time infectious viruses are shed and the number which are shed in any one day surely both increase with more severe disease.
Here are some charts from:
Kinetics of viral load and antibody response in relation to COVID-19 severity
Yanqun Wang and 44 colleagues
Journal of Clinical Investigation 2020-07-07
https://www.jci.org/articles/view/138759
which show that the shedding of SARS-CoV-2 viruses is proportional to COVID-19 disease severity.
Even without any knowledge of the mechanisms by which 25-hydroxyvitamin D levels affect disease severity of viral shedding, we can reason that in countries far from the equator:
1 - Seasonal variations in UV-B skin exposure lead to higher levels of 25-hydroxyvitamin D in summer-autumn and lower levels in winter-spring.
2 - Low 25-hydroxyvitamin D levels increase disease symptom severity in general - especially in influenza and COVID-19.
3 - Viral shedding is reasonably expected to scale with symptom severity. Wang et al. 2020’s observations confirm this.
4 - Since the quantity of viral shedding varies so much, and is a crucial determinant of transmissibility, we can reliably conclude that winter-spring seasonal variations in 25-hydroxyvitamin D, in the absence of robust vitamin D3 supplementation to attain high levels all year round, is a strong driver of transmissibility.
5 - Since transmissibility, for any given level of adaptive immunity in all the individuals in a population, is the primary determinant of how many people are infected in a given time period, we can reliably conclude that, in the absence of robust vitamin D3 supplementation to attain high levels all year round, winter-spring seasonal variations in 25-hydroxyvitamin D levels play a very large role in the total number of people who become infected.
6 - Once infected, disease severity - and so the overall rates of suffering, harm and death - are strongly affected by the effectiveness of any early or late treatments, the most important of which, in the absence of robust vitamin D3 supplementation to attain high levels all year round, is rapid boosting of 25-hydroxyvitamin D above typically low levels such as 5 to 25 ng/mL (12.5 to 37.5 nmol/L) to at least the 50 ng/mL 125 nmol/L level the immune system needs to function properly. nutritionmatters.substack.com/p/calcifediol-to-boost-25-hydroxyvitamin
7 - In the long term, over years and decades, the harm caused by infectious diseases is reduced to the extent that adaptive immune responses to prior infections provide lasting protection against the same or similar pathogens. Higher 25-hydroxyvitamin D levels, by increasing immune system competency, provides such protection to each individual.
8 - To the extent which most or all people in a population properly supplement vitamin D3 to attain at least 50 ng/mL 125 nmol/L 25-hydroxyvitamin D levels, multiple benefits ensue regarding infectious diseases such as influenza and COVID-19, including:
Somewhat reduced chance of being infected for any given viral insult, depending on prior immunity.
If infected, reduced disease severity, which reduces harm and the risk of death and increase the chance that there will be few or no symptoms.
If infected, reduced viral shedding, which benefits all those currently uninfected by reducing the rate of transmission. Ideally this results in R0 [WP] below 1.0 so any outbreaks of infection tend to die out.
If infected, each individual’s long-term immunity is strengthened regarding the specific pathogen and variants of the one which caused the initial infection.
With highly infectious diseases in which sterilising immunity (which completely prevents infection) does not last a lifetime, and which may fade over periods such as months or a few years - as is the case for influenza and COVID-19 - all-year-round high 25-hydroxyvitamin D levels ensure good immune system competency and prevent the seasonal development of the generally low community immune competency which enables the winter-spring seasonal epidemic outbreaks which currently drive most influenza infection.
The same pattern of winter-spring seasonality would be more clearly observed with COVID-19 if its variants settled down into changes with avoid pre-existing immunity to some degree without drastically increasing transmissibility. The recent rapid increases in transmissibility with Alpha, Delta and now especially Omicron variants and sub-variants has created new infection waves even at times of seasonally somewhat elevated 25-hydroxyvitamin D levels.
While we can’t be sure that any given level of 25-hydroxyvitamin D and availability of early treatments will thwart epidemic transmission of future SARS-CoV-2 variants, it is obvious that we should do all we can to boost 25-hydroxyvitamin D levels since this is the simplest, safest, least expensive measure we can take to protect against this and numerous other diseases.











I do not see how to subscribe to your substack
Hi-
I must ask you a stark question. Do the Chinese have lower D3 levels than Europeans and European- Americans? This is the claim of the man who made the Woo Flux video that can be found at bitchute.com. YouTube too, but has been buried by YouTube. Tune in at the 56 minute mark.
Summary --- He says Covid was an intentional release. The Chinese assumed that others worldwide have the same low D3 levels that the Chinese have. That Covid would have been much worse in the USA-Europe if our D3 levels were the same as the Chinese. He says get your D3 up to 90, then the worst that Covid can do to you, is you are sick at home for a few days.
The Chinese defense against Covid would be the very authoritarian isolation measures that only their government can pull off. I only read this once, and months ago. That the Chinese Government was making huge quantities of vitamin C and distributing it. To nullify Covid-19. I obviously can not say true or false on this.
Woo Flux man is Clif_High, who got in very early on bitcoin. He says the same thing about D3 and Covid seasonality.